A Spotlight on Second Opinions After Rita Wilson’s Diagnosis
Keith Kaplan, MD, Chief Medical Officer
News of Rita Wilson’s announcement that she had breast cancer and underwent a double mastectomy has been spreading across media and social media outlets. Anytime a celebrity, vis-à-vis Angelina Jolie or Suzanne Summers or Edie Falco (who played the fictional wife to Tony Soprano) makes public their diagnosis and treatment, the popular media has an opportunity to share their stories with millions of women. Their support promotes breast cancer awareness and early diagnosis and treatment via their publications or on air.
So what does Tom Hank’s wife being diagnosed with breast cancer have to do with pathology? It turns out, a lot. According to media reports in interviews by Mrs. Wilson, she reportedly was originally diagnosed with having lobular carcinoma in-situ (LCIS), a pre-invasive, but not malignant, diagnosis.
As many readers are likely aware, JAMA recently published a study conducted with multiple pathologists in multiple locations and compared their diagnoses with “expert” diagnoses, which in and of themselves, on initial independent review had a 75% concordance among the three experts compared to the “gold standard” or “ground truth” diagnosis. This publication largely looked at concordance among pathologists between clearly benign, clearly malignant and atypical ductal hyperplasia (ADH) and ductal carcinoma in-situ (DCIS) and showed less than 50% agreement among participant pathologists as being able to classify ADH and DCIS.
As I have mentioned elsewhere, this is not new news. Discordant diagnoses in breast as well as other sub-specialty areas of pathology are well known. Recommendations regarding peer review for negative prostate biopsy reads, new malignant diagnoses, high-grade dysplasia in Barrett’s esophagus and grading in astrocytic brain tumors are common in many laboratories given known intra- and inter-observer differences in these as well as other tissue/specimen types.
Mrs. Wilson makes a point of the necessity for double mastectomy arose when her pathology slides were re-reviewed and the original diagnosis of LCIS included invasive carcinoma as well. She is now advocating for second opinions. She is quoted as saying “I am recovering and most importantly, expected to make a full recovery. Why? Because I caught this early, have excellent doctors and because I got a second opinion,” Wilson said. “You have nothing to lose if both opinions match up for the good, and everything to gain if something that was missed is found, which does happen. Early diagnosis is key.”
So where does this leave pathology and pathologists? Are we all going to be expected to get “two sets of eyes” on, at least for starters, breast biopsies and potentially “outside” second opinions amongst ourselves for our patients?
Will pathologists who sign-out breast biopsies be required to obtain fellowship training and additional certification and potentially still be required to share cases? And who determines which cases need to be shared? Lastly, who pays for all this?
These are all questions that I think have been discussed among professional societies, organizations and practices across the country. It is time to address the issue and be on the forefront rather than responding to it when the news breaks.
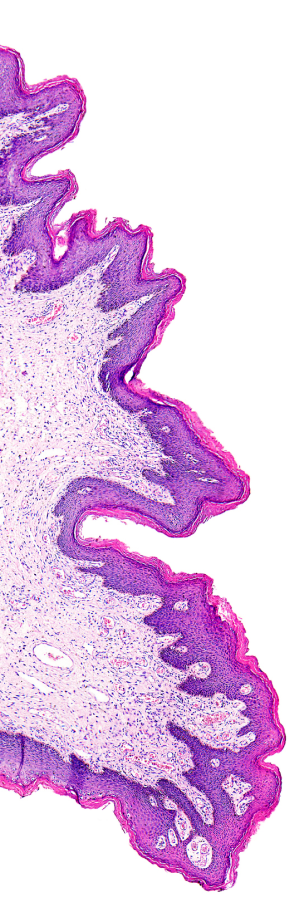
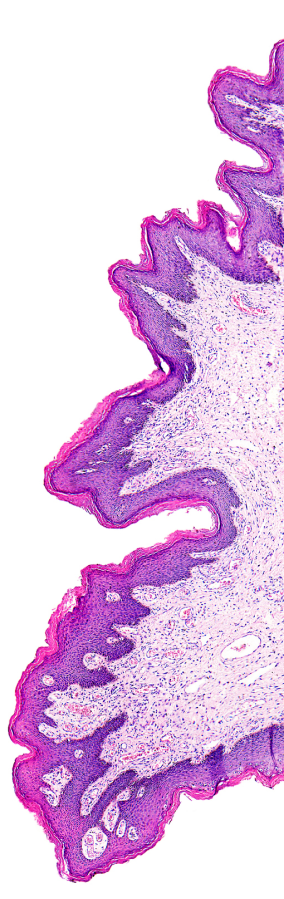
Pathology is not linear, but we try to make it linear. Tumors do not jump from benign to atypical to in-situ to malignant with ability to metastasize. Rather, there are subtle changes that occur over time we try to interpret morphologically based on a subset of tumor cells when the biopsy is performed. It is not always “black and white”, it is often times many shades of gray.
It would seem to be for everyone involved in helping to assess millions of mammograms and breast biopsies performed every year in this country that digital pathology can be an enabling technology to facilitate what may be called “over reads” or “peer review” to ensure quality. Digital pathology can facilitate rapid reviews without need or delay for shipping and receipt of report to patient. It will allow referring pathologists to retain the glass slide material while having colleagues extend their reach in a patient-centric workflow rather than solely a pathologist-centric workflow. This will require all of us to validate our digital pathology systems as well as ourselves.

