

Pathology Societies Need to Follow Radiology’s Lead
Keith Kaplan, MD, Chief Medical Officer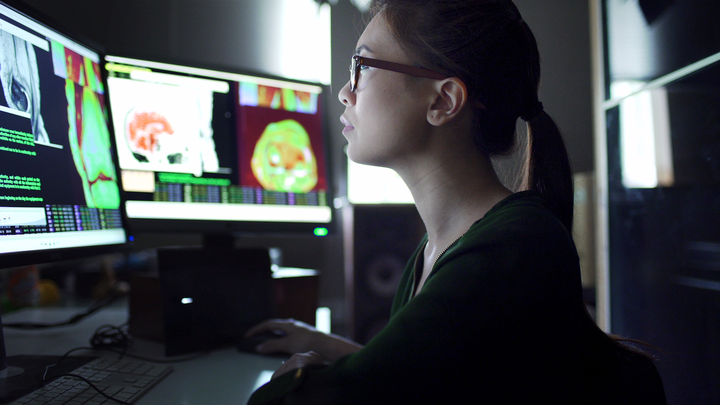
Digital imaging, when most of us consider it in medicine, is primarily used in radiology. Radiology has taken the lead on digital imaging for decades.
When I entered medical school in the early 90’s, printing chest x-rays, mammograms, and CT studies on plastic and holding them up to a light board was the standard of care. But not for long. Before I finished my residency (experimenting with robotic microscopes and video cameras pre-whole slide scanners), “filmless” x-rays and “PACS” entered the discussion. The famous light boards started to find their way into garage sales and medical museums. We have one in our conference room to provide some light to that corner of the room where x-rays use to be shown during tumor boards.
Along the way, radiologists and their societies, drove much of the transformation and standardization. Sure, radiologists moaned and groaned about being filmless and about computers, servers, IT, costs and what it meant to their practice. They voiced their concerns about potential issues with medical care and perhaps even ethical concerns about safety, privacy, access and the like.
Surely not a single radiology department saved any money year one implementing digital radiology. Cost savings and perhaps revenue generation came in later years. Obviously, some of the cost for film and processing solutions has been replaced by costs of servers and monitors and the rest.
Nonetheless, today’s radiologists, those who trained with me in the 90’s, can’t now conceive of a world outside of PACS for viewing their chest x-rays and mammograms and 3-D reconstructions.
Meanwhile, in pathology, our colleges and societies have done little to steer a microscope-free environment and less still to develop standardization or regulation or practice guidelines. A few checklist items (originally written by yours truly) have been the extent of recent efforts. We have failed to keep any committee or special interest group going at the American Telemedicine Association. Our academic societies still pride themselves on multi-head microscope sessions with video monitors.
Perhaps we are better off with analog. All of these organizations and societies and a generation of pathologists can’t be that wrong. Right?
Perhaps digital pathology, unlike digital radiology, has more limited use cases than the institution-wide PACS and the radiologist’s light board and “hot lamp”-free work zones?
But what are those use cases?
Radiology societies and thought leaders have put out use cases for artificial intelligence in radiology, once again, in my opinion, leading the way and setting an example for other specialties. Pathology, as the other image-intense specialty, could be doing the same, guiding researchers towards probable use cases and getting clinicians to think about how to work smarter, not harder.
Per the American College of Radiology: “In order to foster standardized, safe and effective AI for clinical decision support and diagnostics, the American College of Radiology Data Science Institute (ACR DSI) has released a number of high-value use cases for artificial intelligence in medical imaging, which will be continuously updated as new opportunities present themselves.”
Identifying cardiovascular abnormalities, detecting fractures and other musculoskeletal injuries, aiding in the diagnosis of neurological diseases, flagging thoracic complications and conditions, and screening for common cancers such as breast and lung and colon top the list of radiology’s use cases.
I don’t see the same trend occurring in pathology, taking advantage of burgeoning deep learning technologies and efforts to “foster standardized, safe and effective AI for clinical decision support and diagnostics”.
When will we as a medical specialty think ahead, not about how technology might eliminate jobs or offshore them or make our work less meaningful or impact reimbursements, but rather to organize ourselves as “new opportunities present themselves"?
